While dozens of variants have spawned from the original COVID-19 virus, health experts say the delta variant is the most transmissible so far. Research also shows it’s leading to higher rates of hospitalization for those infected.
Here’s what you need to know
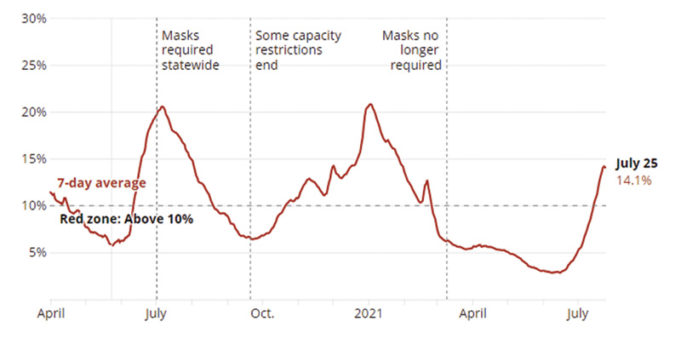
Earlier this month, the state’s positivity rate — the ratio of confirmed cases to tests — went above 10% for the first time since February, a threshold that Gov. Greg Abbott previously identified as dangerous. Statewide, hospitalizations have increased this month as well.
Health officials are also worried about the current stalled vaccination rates in the state and country, which have given the virus room to spread. As of Tuesday, nearly 43% of Texans have been fully vaccinated. The state continues to lag behind the national vaccination rate of 48.8%, according to the Mayo Clinic.
What’s the delta variant of the coronavirus?
Viruses like the coronavirus frequently change by mutating. It’s challenging to know the exact number of variants out there globally or in Texas, health experts say.
Checking for these variants happens by analyzing a random sample of COVID-19 tests, so there is a possibility that some mutations might be missed. With all viruses, some variants eventually disappear while others persist. Only time will tell how different variants will affect people and how extensive they will be. The most effective way to curb new variants is to prevent spreading the virus and avoid giving it a chance to mutate.
That delta variant, known by scientists as B.1.617.2, was first identified in India. It triggered a devastating outbreak there in April and May and has since spread to at least 100 other countries, attacking areas where vaccination rates are the lowest.
Should I wear a mask?
The Texas Department of State Health Services (DSHS) recommends people protect themselves from the delta variant the same way they do for other COVID-19 variants. This includes wearing a multilayered, well-fitted mask covering both the nose and mouth; limiting gatherings with people outside of your household; and getting tested when necessary. Texas health experts have also recommended staying away from people who aren’t following COVID-19 safety protocols.
The Centers for Disease Control and Prevention (CDC) and the World Health Organization (WHO) are encouraging everyone to wear masks while inside. Recently updated guidance from the American Academy of Pediatrics also recommends that all students over 2 years old and school staff continue to wear masks.
Tarrant County Judge Glen Whitley has signed a declaration of local disaster to help contain the spread of the virus, and on Friday, Dallas County raised its threat level to orange, or “extreme caution,” which urges unvaccinated people to avoid large crowds, among other guidance. Austin and Travis County officials are encouraging vaccinated people to wear masks indoors and outdoors and telling unvaccinated people to stay home except for essential needs. On Thursday, Harris County’s emergency threat level was raised to orange — or “significant.” Harris County Judge Lina Hidalgo called for people to continue wearing masks as cases begin to increase.
However, these and any other local guidelines in Texas have no weight of law behind them because Abbott banned local pandemic mandates. The governor said Wednesday that he will not impose another statewide mask mandate. He lifted the statewide mask requirement in March which had been in place since the summer of last year. Texas schoolchildren will not face mask requirements as they return to school later this summer.
How else should I protect myself?
If you’re able to, health experts say the best thing to do is to get fully vaccinated against COVID-19.
The CDC also recommends avoiding poorly ventilated venues and large crowds, washing your hands often, covering your coughs and sneezes, cleaning and sanitizing highly touched surfaces daily, and monitoring your health daily. Texas health experts have also recommended staying away from people who aren’t following COVID-19 safety protocols.
How contagious is the delta variant?
Proteins on the outer spikes of the delta variant are “stickier,” making it more transmissible than other variants, said Dr. Katelyn Jetelina, an epidemiologist at the University of Texas School of Public Health in Dallas. Studies have shown that the delta variant is up to 60% more transmissible than the previous leading variant, the alpha variant. A study from Scotland found that the hospitalization rate of those who contracted the delta variant was about 85% higher than those fighting the alpha variant.
The variant’s symptoms are more similar to those of a cold — headaches, sore throat, runny nose, and fevers — than common COVID-19 symptoms such as coughing and loss of smell, according to the COVID Symptom Study, a project by doctors and scientists to track the symptoms and spread of the virus.
Fully vaccinated people can and have gotten COVID-19. However, these cases are overwhelmingly asymptomatic or mild. These types of cases are known as “breakthrough infections,” but experts say they are uncommon. Fully vaccinated people who become seriously ill, hospitalized, or die are even rarer, reports The New York Times, but this also means that vaccinated people may spread COVID-19 to others.
Will the vaccine protect me?
According to Yale Medicine, the Pfizer-BioNTech vaccine is 88% effective against symptomatic cases of the delta variant and 96% effective against hospitalizations. Researchers are still studying the efficacy of the Moderna vaccine against the delta variant but believe it may work similarly to Pfizer’s. The Johnson & Johnson vaccine also retains much of its efficacy against the delta variant at around 60%, according to recent research.
Current data show the people who are at most risk are the unvaccinated. No vaccine is 100% effective at preventing the spread of a virus, but studies and research have shown that the COVID-19 vaccines are effective at reducing the risk of serious illness.
Reuters reports that 97% of people entering hospitals in the United States with COVID-19 are unvaccinated. Nationwide, deaths are up 26%, with outbreaks occurring in parts of the country with low vaccination rates, according to the CDC earlier this month.
Since early February, 8,787 people have died in Texas due to COVID-19. At least 43 were fully vaccinated. That means 99.5% of people who died due to COVID-19 in Texas from Feb. 8 to July 14 were unvaccinated, while 0.5% were the result of “breakthrough infections,” which the DSHS defines as people who contracted the virus two weeks after being fully vaccinated.
These breakthrough infections are rare, according to health experts, but some worry the small percentage of fully vaccinated people who do end up getting the virus could develop “long COVID,” a poorly understood group of symptoms that people experience four or more weeks after first being infected with the virus.
Who’s eligible for the vaccine?
All people 12 and older are eligible for the COVID-19 vaccine in Texas. Children ages 12-17 can get the Pfizer vaccine, but COVID-19 vaccines are not mandatory for Texas students.
Based on several factors, medical experts believe the COVID-19 vaccines are safe and effective even for the medically vulnerable, but several studies are in the works, including trials and research happening in Texas, to deepen scientific understanding of how the vaccines affect people with immune disorders; cancer and transplant patients who are taking immunosuppressant medications; and people who have allergies.
State and local health officials say that vaccine supply is healthy enough to meet demand across much of Texas. Most chain pharmacies and many independent ones have a ready supply of vaccine doses, which is administered free and mainly on a walk-in basis. Many private doctors’ offices also have doses. And you can check current lists of large vaccine hubs that are still operating here.
Public health departments also have vaccines. You can register with the Texas Public Health Vaccine Scheduler either online or by phone, and businesses or civic organizations can set up vaccine clinics to offer it to employers, visitors, customers, or members.
Medical experts recommend that people who have had COVID-19 should still get the vaccine. If someone’s treatment included monoclonal antibodies or convalescent plasma, they should talk to their doctor before scheduling a vaccine appointment. The CDC recommends that people who received those treatments should wait 90 days before getting the vaccine.
A version of this story originally appeared in the Texas Tribune.